Ný rannsókn sýnir annað tilfelli af farsælli HIV sjúkdómshléi eftir beinmergsígræðslu
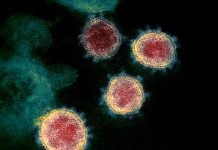
Að minnsta kosti ein milljón manna deyja af HIV-tengdum orsökum á hverju ári og tæplega 35 milljónir búa við HIV. HIV-1 (Human Immunodeficiency Virus) ber ábyrgð á meirihluta HIV sýkinga um allan heim og smitast með beinni snertingu við HIV sýktan líkamsvessa. Veiran ræðst á og drepur mikilvægar frumur sem berjast gegn sýkingum í ónæmiskerfi okkar. Það er engin lækning við HIV. Eins og er er aðeins hægt að meðhöndla HIV með því að nota lyf sem hafa getu til að bæla HIV veira. These drugs have to be taken life long and it is challenging plus a cost burden on the health system especially in low-and-middle-income countries. Only 59 percent of patients of HIV worldwide are receiving Antiretroviral therapy (ARV) and HIV virus is fast becoming resistant from many known drugs which itself is a major concern.
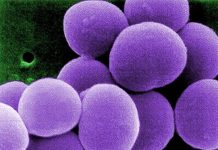
Beinmergsígræðsla (SÞ) is a treatment used for leukemia, myeloma, lymphoma etc. Bone marrow, the soft tissue inside bones, makes blood-forming cells including the infection fighting white blood cells. A bone marrow transplant replaces unhealthy marrow with a healthy one. In the first case of successful HIV remission, an HIV-infected individual called ‘Berlin Patient’ who later revealed his name received a bone marrow transplant a decade ago when he was targeted to treat acute leukemia. He received two transplants along with total body irradiation which led to long-term HIV eftirgjöf.
Í nýrri rannsókn sem birt var í Nature led by UCL and Imperial College London, the only second person has been shown to experience sustained remission from HIV-1 after a bone marrow transplant and stoppage of treatment. The anonymous adult male patient from UK was diagnosed with HIV infection in 2003 and was on antiretroviral therapy treatment since 2012. He was subsequently diagnosed with Hodgkin’s Lymphoma in the same year and he underwent chemotherapy. In 2016, he was given stem cell transplant from a donor who carried a genetic mutation which prevents expression of a most commonly used HIV receptor protein called CCR5. Such a donor is resistant to HIV-1 strain of the virus which specifically uses CCR5 receptor and thus the virus now cannot enter host cells. Since chemotherapy kills cells which are dividing, HIV could be targeted. From this understanding if one’s immune cells are replaced by cells which do not have CCR5 receptor, HIV can be prevented from rebounding after the treatment.
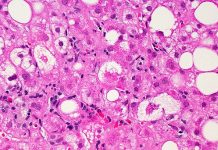
Ígræðslan var framkvæmd með minniháttar aukaverkunum eins og vægum fylgikvilla sem er algengur í ígræðslu þar sem ónæmisfrumur viðtakanda verða fyrir árás á ónæmisfrumur gjafa. Andretróveirulyfjameðferð var haldið áfram í 16 mánuði eftir ígræðsluna áður en tekin var ákvörðun um að hætta meðferð til að meta bata HIV-1. Eftir þetta hélt veiruálag sjúklingsins áfram að vera ógreinanlegt. Sjúklingurinn var í sjúkdómshléi eftir 18 mánuði eftir að andretróveirumeðferð var stöðvuð þar sem ónæmisfrumur sjúklingsins gátu ekki framleitt mikilvægan CCR5 viðtaka. Þessi heildarlengd jafngildir 35 mánuðum eftir ígræðslu.
This is a second case of a patient exhibiting sustained remission of HIV-1 following a bone marrow transplant. One important difference in this second patient being that ‘Berlin Patient’ had received two transplants along with total body irradiation while this UK patient received only a single transplant and underwent less aggressive and lesser toxic approach of chemotherapy. Mild complications of similar nature were seen in both patients i.e. graft versus host disease. Achieving success in two different patients points towards developing strategies based on preventing CCR5 expression which might even cure HIV.
Authors state that they are monitoring the patient’s condition and cannot say with affirmation yet if he has been cured of HIV. This may not be a generalized appropriate treatment for HIV because of adverse effects and toxicity of chemotherapy. Also, bone-marrow transplants are expensive and carry risks. Nevertheless, it is a better approach with reduced intensity conditioning and no irradiation. Research could also focus on knocking out the CCR5 receptor using gene therapy in people with HIV.
***
{Þú getur lesið upprunalegu rannsóknarritgerðina með því að smella á DOI hlekkinn sem gefinn er upp hér að neðan á listanum yfir tilvitnaðar heimildir}
Heimildir)
1. Gupta RK o.fl. 2019. HIV-1 sjúkdómshlé eftir CCR5Δ32/Δ32 blóðmyndandi stofnfrumuígræðslu. Náttúran. http://dx.doi.org/10.1038/s41586-019-1027-4
2. Hütter G. o.fl. 2009. Langtímastjórnun á HIV með CCR5 Delta32/Delta32 stofnfrumuígræðslu. N Engl J Med. 360. https://doi.org/10.1056/NEJMoa0802905
3. Brown TR 2015. I Am the Berlin Patient: A Personal Reflection', AIDS Research and Human Retroviruses. 31(1). https://doi.org/10.1089/aid.2014.0224